Recently, the ESHRE journal Human Reproduction published the study of Spangmose et al. “Obstetric and perinatal risk in 4601 singletons and 884 twins conceived after fresh blastocyst transfers: a Nordic study from the CoNARTaS group” (2020 Apr 28;35(4):805-815, doi: 10.1093/humrep/deaa032). Although the title does not describe authentically, the study has compared outcomes of fresh blastocyst transfers with those after cleavage-stage transfer and spontaneous conception. Authors have found that fresh blastocyst transfer is associated with a higher risk of placental and perinatal complications, including placenta previa and preterm birth. Additionally, blastocyst transfer has altered male/female ratio with more males, and the risk of same-sex twins after single blastocyst transfer compared with single cleavage-stage embryo transfer. Authors concluded that the extended embryo culture to the blastocyst stage has the potential to compromise obstetric and perinatal outcomes in fresh cycles. This conclusion published in a prominent journal might have long-term impacts on the ongoing debate in the issue, providing a serious argument to reverse the actual tendency, as many clinics may prefer to remain at or return to the “seemingly safer” D2-3 transfer.
But were these data carefully investigated, were all possible factors considered and is the conclusion entirely justified?
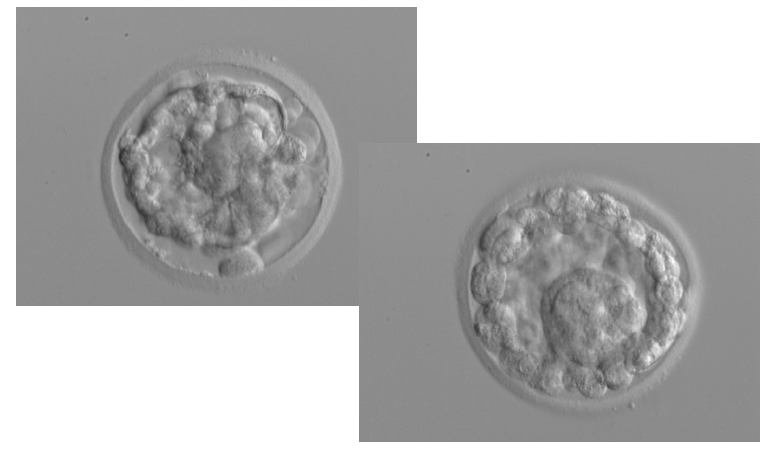
In our letter to the Editor (Vajta and Parmegiani, Cleavage stage vs. blastocyst transfer: a more considerate analysis suggested; Human Reproduction in press, doi: 10.1093/humrep/deaa202), we highlighted the following facts. Blastocyst culture is a relatively new technology that has been introduced slowly after the millennium worldwide. During the initial years of the study of Spangmose et al., blastocyst culture and transfer were still at the starting period, with wrong gas composition, inappropriate media, and embryo handling issues. Up till today, many clinics use 5% carbon dioxide in air mixtures, although there is a more than 20-years old evidence that the high oxygen concentration is detrimental for in vitro growing embryos. Despite significant advancement, there are many misunderstandings regarding the optimal use of appropriate media. The recent focus on lack of proper humidification of many commercially available incubators might also compromise the outcome of blastocyst cultures. Culture to the blastocyst stage requires longer in vitro periods, and all negative effect may be amplified. Additionally, lack of standardisation and eclectic – randomly used protocols may also have a long-term influence on development.
However, these problems are not intrinsic components of blastocyst culture, just consequences of its inappropriate application.
On the other hand, the benefits of fresh blastocyst-stage transfer are obvious: higher pregnancy and birth rates. These data should have been mentioned first, followed with the concerns created by a very slight increase in adverse outcomes, and factors possibly contributing in these negative effects should be listed, or – preferably – analysed where applicable.
Our final conclusion was: instead of throwing the baby out with the bathwater and considering a return to the cleavage-stage transfer, we should do our best to improve and standardise our blastocyst culture technique by eliminating systematically factors that cause complications.
In their Reply to our letter (Spangmose and Pinborg, Human Reproduction, in press,
doi: 10.1093/humrep/deaa201) authors agreed that they could have emphasised more on blastocyst culture and improvements, but they did not consider to be in the scope to describe the pros and cons of blastocyst culture.
According to the rules of Human Reproduction, with this answer, the debate was closed – obviously only on the pages of the journal.